
The DECIDE Model in Nursing: A Step-by-Step Guide to Effective Decision Making Using the DECIDE Decision-Making Model as a Practical Decision-Making Tool
Clinical practice requires disciplined reasoning, ethical awareness, and the ability to respond appropriately to rapidly changing patient conditions. In modern healthcare environments, decisions are rarely simple; they often involve incomplete data, competing priorities, and significant consequences. Within this context, decision making becomes a central professional responsibility rather than a routine task. The DECIDE Model in Nursing offers a structured, systematic framework that supports clinicians in navigating complex situations with clarity, accountability, and analytical precision.
The DECIDE Model in Nursing is recognized as a comprehensive decision-making model designed to guide practitioners through a logical and organized decision-making process. Rather than relying solely on intuition or fragmented reasoning, the model encourages a deliberate, step-by-step progression through clearly defined stages. This structured approach reduces ambiguity, promotes consistency, and supports effective decision making in environments where errors can compromise patient safety.
At its core, the DECIDE Model in Nursing is built around an acronym of 6 particular activities needed to guide clinical reasoning. The decide model is the acronym that represents these sequential cognitive steps, each functioning as a deliberate checkpoint within the broader decision-making process called DECIDE. The model ensures that practitioners define the problem accurately, consider possible solutions, establish the criteria for selecting among alternatives, and evaluate outcomes after implementing the decision. By following this systematic approach, nurses are better positioned to make informed decisions rather than reactive choices.
Healthcare decisions frequently involve sensitive information, ethical implications, and a number of options that must be weighed carefully. Without a structured framework, the risk of making the wrong decision increases, particularly under time pressure. The DECIDE Model in Nursing offers a structured way to approach complex decisions by organizing thought processes into manageable and logical stages. Research on clinical judgment and cognitive reasoning consistently emphasizes that systematic approaches improve diagnostic accuracy and reduce cognitive bias (Tanner, 2006; Croskerry, 2009). By promoting analytical reflection, the model supports effective decisions that align with professional standards and evidence-based practice.
The relevance of the DECIDE Model in Nursing extends beyond bedside care. It serves as a decision-making tool in leadership contexts, interdisciplinary collaboration, and quality improvement initiatives. Much like business leaders evaluating strategic options before determining the best course of action, healthcare professionals must analyze available evidence, patient preferences, and institutional policies before implementing a plan of action. In this way, the model provides a disciplined framework for evaluating the outcome of decisions and refining future practice.
Importantly, the DECIDE Model in Nursing does not function as a rigid formula. Instead, it offers a flexible yet systematic approach that adapts to diverse clinical settings, from acute care to community health environments. The model provides clarity when navigating uncertainty, ensuring that every decision reflects critical thinking, ethical reasoning, and accountability. By encouraging practitioners to evaluate and monitor results, it reinforces a culture of continuous improvement and reflective practice.
This discussion provides a comprehensive exploration of the DECIDE Model in Nursing, examining its conceptual foundation, its role in supporting effective decision-making, and its practical application in real-world healthcare settings. Through an in-depth analysis of each step of the decision-making process, the guide demonstrates how structured reasoning enhances clinical judgment and strengthens professional accountability. Ultimately, the DECIDE Model in Nursing offers a systematic framework for making informed choices in environments where thoughtful, evidence-based decisions are essential to patient safety and quality care.
Understanding the DECIDE Model as a Decision-Making Tool in Nursing
The DECIDE Model in Nursing is widely regarded as a structured approach to the decision-making process that strengthens clinical judgment and promotes professional accountability. In complex healthcare environments where decisions are made under pressure, a systematic framework offers clarity and direction. The DECIDE Model in Nursing functions as a practical decision-making tool that organizes reasoning into logical, sequential steps, ensuring that every decision is deliberate rather than impulsive.
At its core, the DECIDE Model in Nursing is built around an organized cognitive pathway often referred to as the decide decision-making framework. This decision-making process called DECIDE emphasizes careful analysis before action. By guiding practitioners through defined stages, the model ensures that choices are aligned with patient needs, ethical standards, and available evidence. It offers a structured method for approaching situations that involve uncertainty, multiple variables, and a number of options requiring evaluation.
Importantly, the model provides more than theoretical guidance; it offers a structured way to approach real clinical challenges. Whether addressing medication discrepancies, prioritizing patient care in a high-acuity unit, or responding to ethical dilemmas involving sensitive information, the DECIDE Model in Nursing promotes disciplined reasoning. This structured approach reduces the likelihood of making the wrong decision and enhances effective decision making in high-stakes environments.
Using the D.E.C.I.D.E Acronym to Structure Clinical Decision Making
DECIDE Model Is the Acronym Explained Clearly
The DECIDE Model in Nursing is grounded in a clearly defined acronym of 6 particular activities that guide the decision-making process. The decide model is the acronym that represents the following six particular activities needed for sound reasoning:
- D – Define the problem
- E – Establish the criteria
- C – Consider possible solutions
- I – Identify the best alternative
- D – Develop and implement a plan
- E – Evaluate and monitor the outcome
Each step of the decide model functions as a deliberate cognitive checkpoint within the broader decision-making process. By using the D.E.C.I.D.E sequentially, practitioners ensure that reasoning remains organized and comprehensive. The framework is designed to promote effective decisions by encouraging careful evaluation before and after action.
This acronym-based structure enhances clarity. Rather than relying on fragmented thought processes, clinicians follow a logical progression that supports consistent reasoning across various settings. The DECIDE Model in Nursing therefore acts as a reliable guide for navigating complex decisions in patient care.
Breakdown of the Six Stages in Sequence
The effectiveness of the DECIDE Model in Nursing lies in its sequential design. Each stage builds upon the previous one, reinforcing a systematic approach to clinical reasoning.
- Define the problem
The first step of the decision-making process requires accurate identification of the issue. For example, a patient presenting with shortness of breath may initially appear anxious; however, defining the problem requires assessing oxygen saturation, respiratory rate, and underlying conditions to determine whether the root cause is hypoxia, pulmonary embolism, or anxiety. - Establish the criteria
Once the problem is defined, clinicians establish the criteria for selecting interventions. These criteria may include patient safety, urgency, evidence-based guidelines, and ethical considerations. - Consider possible solutions
This stage involves generating a number of options. In the case of deteriorating oxygen saturation, possible solutions may include oxygen therapy, repositioning, diagnostic imaging, or medication administration. - Identify the best alternative
Through risk-benefit analysis and evidence appraisal, the clinician selects the best alternative that aligns with established criteria. - Develop and implement a plan
The chosen intervention is translated into a clear plan of action. This includes delegation, documentation, and communication with interdisciplinary teams. - Evaluate and monitor outcomes
The final step involves evaluating the outcome to determine effectiveness. If the patient’s oxygen saturation improves, the intervention is validated; if not, the process may cycle back to reassessment.
By following these six stages, the DECIDE Model in Nursing offers a structured way to approach clinical reasoning that reduces ambiguity and enhances clarity.
Why Structured Decision Making Improves Patient Safety
Structured decision making improves patient safety by minimizing cognitive errors and promoting accountability. Research on diagnostic reasoning indicates that systematic approaches reduce biases such as anchoring and premature closure (Croskerry, 2009). When practitioners rely solely on intuition, they risk overlooking critical data. However, the DECIDE Model in Nursing encourages deliberate analysis at each step of the decision-making process.
For example, consider medication administration. Without a structured framework, a practitioner might proceed based on assumption. Using the DECIDE Model in Nursing ensures that the problem is clearly defined (e.g., medication discrepancy), criteria are established (patient safety and dosage accuracy), and outcomes are evaluated after implementing the decision. This systematic approach strengthens safe practice standards and enhances effective decision-making across clinical contexts.
Why the DECIDE Model Supports Effective Decision Making in Complex Clinical Situations
Clinical Judgment and Accountability
Clinical judgment involves interpreting patient data, anticipating complications, and selecting the best course of action. The DECIDE Model in Nursing strengthens this judgment by promoting a disciplined reasoning pathway. Because decisions are made transparently within a structured framework, accountability is reinforced. Each step of the decision-making process can be justified and documented, supporting professional standards and ethical responsibility.
In high-acuity settings such as emergency departments or intensive care units, rapid yet accurate reasoning is essential. The DECIDE Model in Nursing ensures that even urgent decisions follow a systematic approach rather than reactive impulses.
Reducing Errors Through Systematic Reasoning
Healthcare errors often arise from fragmented reasoning or incomplete data analysis. The DECIDE Model in Nursing reduces these risks by encouraging systematic reasoning. By requiring clinicians to evaluate multiple possible solutions before selecting the best alternative, the model minimizes oversight and enhances effective decision making.
For instance, when managing postoperative pain, practitioners must balance analgesic effectiveness with potential side effects. A structured approach ensures careful consideration of patient history, allergies, and risk factors before implementing the decision.
Evidence-Based Practice Integration
The DECIDE Model in Nursing aligns closely with evidence-based practice principles. During the stage of establishing criteria and identifying the best alternative, clinicians integrate research findings, clinical guidelines, and patient preferences. This integration ensures that decisions are not only logical but also supported by current evidence.
Define the Problem Clearly in the Decision-Making Process
The first and arguably most critical step of the DECIDE Model in Nursing is to define the problem with precision and clarity. Within any structured decision-making process, inaccurate problem identification compromises every subsequent step. If the foundation is flawed, even well-executed later stages—such as selecting a best alternative or implementing a plan of action—may lead to ineffective or unsafe outcomes.
The DECIDE Model in Nursing emphasizes that defining the problem is not merely stating a symptom; it is a deliberate act of analytical reasoning. This stage of the decision-making process called DECIDE requires clinicians to differentiate between observable manifestations and the underlying issue driving them. In high-stakes environments, where time constraints and patient acuity demand rapid judgment, a structured approach prevents reactive thinking and strengthens effective decision making.
By clearly defining the problem at the outset, the DECIDE Model in Nursing ensures that every subsequent step of the decision-making process is aligned with accurate clinical understanding. This systematic approach reduces variability in decisions made and strengthens patient safety outcomes.
How to Define the Problem Accurately in Clinical Practice
Gathering Relevant Data
Accurate problem identification begins with comprehensive data collection. Within the DECIDE Model in Nursing, defining the problem involves gathering subjective and objective information before attempting to make a decision. This includes:
- Vital signs and physical assessment findings
- Laboratory and diagnostic results
- Patient history and current medications
- Psychosocial and environmental factors
- Communication from interdisciplinary team members
For example, consider a patient presenting with confusion. Without structured analysis, one might prematurely attribute the condition to age-related cognitive decline. However, using the DECIDE Model in Nursing, the clinician gathers relevant data: electrolyte levels, oxygen saturation, medication changes, infection markers, and recent surgical history. This broader evaluation may reveal hypoxia or sepsis rather than dementia as the root cause.
Systematic data collection supports a structured approach to reasoning and minimizes reliance on assumptions. Research in clinical judgment underscores that incomplete data gathering is a leading contributor to diagnostic error (Tanner, 2006; Croskerry, 2009). By embedding thorough assessment into the first step of the decision-making process, the model ensures that reasoning is grounded in evidence rather than speculation.
Distinguishing Symptoms from Root Causes
A central principle of the DECIDE Model in Nursing is differentiating between symptoms and underlying causes. Symptoms are often visible and immediate; root causes require deeper analysis. Failure to distinguish between the two may result in addressing surface manifestations rather than the true clinical issue.
For instance, a postoperative patient reports severe pain. The symptom is pain, but the root cause may vary: inadequate analgesia, surgical complication, anxiety, or infection. Through systematic reasoning, clinicians examine wound integrity, vital signs, drainage, and medication timing before identifying the most plausible explanation.
In this context, the DECIDE Model in Nursing reinforces diagnostic reasoning by encouraging careful evaluation of multiple possible solutions before moving forward in the decision-making process. This disciplined reasoning strengthens effective decisions and prevents fragmented care.
Avoiding Premature Conclusions
Premature closure—settling on a diagnosis or explanation without adequate analysis—is a well-documented cognitive bias in healthcare. The DECIDE Model in Nursing mitigates this risk by requiring deliberate progression through each step of the decision-making process.
For example, a patient experiencing chest discomfort might initially appear to have musculoskeletal pain. However, if the clinician prematurely concludes this without evaluating cardiac risk factors, electrocardiogram findings, and troponin levels, the consequences could be severe.
By intentionally pausing to define the problem accurately, the DECIDE Model in Nursing promotes reflective thinking. It discourages reactive responses and supports a systematic approach to complex decisions. Avoiding premature conclusions strengthens accountability and enhances patient safety.
The Impact of Problem Definition on Effective Decisions
Diagnostic Reasoning
Defining the problem accurately directly influences diagnostic reasoning. The first step of the decision-making process shapes how clinicians interpret data, prioritize interventions, and identify the best course of action. If the problem is misidentified, subsequent criteria and chosen interventions may not address the true clinical need.
The DECIDE Model in Nursing integrates diagnostic reasoning into its framework by ensuring that clinicians thoroughly analyze presenting concerns before proceeding. This enhances the quality of decisions made and supports effective decision-making across diverse clinical settings.
For example, in community health practice, a rise in patient readmissions might initially appear to be a compliance issue. However, careful problem definition may reveal socioeconomic barriers, limited access to transportation, or medication affordability challenges. Addressing the root cause rather than the superficial symptom results in more sustainable and patient-centered outcomes.
Consequences of Misidentifying the Problem
The consequences of incorrectly defining the problem can be significant. These may include:
- Delayed treatment
- Increased healthcare costs
- Medication errors
- Patient dissatisfaction
- Adverse outcomes
In acute care, misinterpreting early signs of sepsis as mild infection may delay life-saving interventions. In leadership contexts, misidentifying staffing shortages as performance deficiencies may result in ineffective policy changes.
The DECIDE Model in Nursing reduces the risk of making the wrong decision by reinforcing structured analysis at the outset. When clinicians follow a disciplined framework, they are better positioned to make informed decisions and ensure that subsequent interventions align with actual needs.
Real Clinical Examples
Example 1: Acute Care Scenario
A patient presents with hypotension following surgery. If the problem is defined simply as “low blood pressure,” interventions may focus narrowly on fluid administration. However, using the DECIDE Model in Nursing, the clinician gathers additional data: hemoglobin levels, drainage output, heart rate, and surgical site assessment. The root cause may be internal bleeding rather than dehydration. Correctly defining the problem leads to rapid surgical intervention rather than ineffective fluid replacement alone.
Example 2: Medication Safety Scenario
A patient reports dizziness after receiving antihypertensive medication. Without thorough assessment, the problem may be assumed to be medication intolerance. Further evaluation reveals that the dose was administered twice due to documentation error. Defining the problem accurately prevents repeated dosing and supports safer practice.
Example 3: Community Health Scenario
In a public health clinic, rising rates of uncontrolled diabetes might initially be attributed to poor adherence. A deeper problem definition reveals limited health literacy and cultural dietary factors. Interventions then shift toward targeted education rather than punitive measures.

Establish the Criteria for Sound Clinical Decision Making
Within the DECIDE Model in Nursing, once clinicians define the problem accurately, the next critical step of the decision-making process is to establish the criteria that will guide action. This stage ensures that decisions are not based on impulse, habit, or convenience, but instead grounded in measurable standards, professional expectations, and patient-centered goals.
The DECIDE Model in Nursing emphasizes that effective decision making depends on clearly articulated criteria. Without defined standards, even well-intentioned practitioners may struggle to identify the best course of action among multiple possible solutions. Establishing criteria introduces structure into the decision-making process and strengthens accountability. It transforms abstract reasoning into a systematic evaluation of options aligned with safety, ethics, and evidence.
In practice, criteria function as benchmarks against which each potential intervention is measured. They shape how clinicians make informed decisions, especially in complex clinical situations involving uncertainty or competing priorities. By integrating clear benchmarks early in the process, the DECIDE Model in Nursing ensures that every subsequent step remains logically connected to professional standards and patient outcomes.
How to Establish the Criteria for Safe and Ethical Nursing Decisions
Patient-Centered Priorities
Patient-centered care is foundational to sound decision making. Within the DECIDE Model in Nursing, establishing criteria begins by identifying what matters most to the patient. This includes:
- Safety and risk reduction
- Symptom relief
- Functional improvement
- Cultural and spiritual considerations
- Quality of life goals
For example, consider an elderly patient with advanced heart failure who is experiencing shortness of breath. While aggressive interventions may be available, patient-centered criteria might prioritize comfort and dignity over invasive procedures. In this case, establishing criteria rooted in patient values shapes how clinicians approach the decision-making process.
The DECIDE Model in Nursing reinforces that decisions are not made in isolation from individual needs. By explicitly integrating patient-centered priorities, clinicians avoid making the wrong decision based solely on clinical indicators without considering personal preferences.
Clinical Guidelines and Protocols
Evidence-based clinical guidelines provide objective standards that inform the decision-making process. When practitioners establish criteria within the DECIDE Model in Nursing, they draw from:
- Institutional protocols
- National practice guidelines
- Evidence-based recommendations
- Safety checklists
For instance, when managing sepsis, established protocols outline criteria such as timely antibiotic administration, fluid resuscitation parameters, and laboratory monitoring. By aligning decision criteria with recognized standards, clinicians strengthen effective decision-making and ensure consistency in care delivery.
Clinical guidelines also reduce variability in decisions made across providers. Research in evidence-based practice consistently demonstrates that structured frameworks improve patient outcomes and reduce preventable complications (Melnyk & Fineout-Overholt, 2019). Within the DECIDE Model in Nursing, guidelines serve as anchors that ground reasoning in validated evidence.
Ethical and Legal Considerations
Sound clinical reasoning must account for ethical and legal responsibilities. Establishing criteria involves examining:
- Patient autonomy
- Beneficence and nonmaleficence
- Confidentiality and protection of sensitive information
- Legal scope of practice
- Documentation requirements
For example, when a patient refuses a recommended treatment, the clinician must balance beneficence with respect for autonomy. The DECIDE Model in Nursing encourages structured evaluation of ethical dimensions before moving forward in the decision-making process.
Legal considerations also influence criteria. Administering treatment outside professional scope or failing to obtain informed consent can lead to serious consequences. By incorporating ethical and legal benchmarks early, the model ensures that decisions are defensible, accountable, and aligned with regulatory standards.
Prioritizing Criteria to Identify the Best Possible Outcome
Once criteria are established, the next task within the DECIDE Model in Nursing is prioritization. In many clinical situations, multiple criteria compete for attention. Effective decision making requires ranking these factors according to urgency, impact, and feasibility.
Weighing Risks and Benefits
Risk-benefit analysis is central to identifying the best possible outcome. Clinicians must examine how each potential intervention aligns with the established criteria.
Consider a patient with atrial fibrillation who requires anticoagulation therapy. The benefits include reduced stroke risk, while the risks involve potential bleeding complications. Within the DECIDE Model in Nursing, the decision maker evaluates both dimensions carefully before determining the best alternative.
Weighing risks and benefits enhances effective decisions by ensuring that no single factor dominates without balanced evaluation. It reinforces a systematic approach to complex decisions, especially when patient safety is at stake.
Resource Considerations
Healthcare decisions often occur within practical constraints. Staffing levels, equipment availability, and financial resources may influence how criteria are prioritized.
For example, in a community health clinic with limited access to advanced imaging, clinicians may need to rely on clinical assessment and laboratory findings to guide interventions. While resource considerations should not compromise safety, they are part of the real-world decision-making process.
The DECIDE Model in Nursing acknowledges that resource allocation is a legitimate factor in establishing and prioritizing criteria. Recognizing these constraints promotes transparency and ensures that decisions remain realistic and sustainable.
Patient Preferences
Patient preferences frequently shape the final determination of the best course of action. Shared decision making strengthens trust and improves adherence to care plans.
For example, a patient with newly diagnosed hypertension may prefer lifestyle modification before initiating pharmacological treatment. When preferences are considered alongside safety criteria and clinical guidelines, clinicians can make informed choices that respect autonomy while maintaining professional standards.
The DECIDE Model in Nursing integrates patient preferences as a formal component of the structured approach to reasoning. This ensures that care remains individualized rather than protocol-driven alone.
Integrating Criteria into the Broader Decision-Making Process
Establishing and prioritizing criteria ensures that the subsequent step of the decision-making process—selecting the best alternative—rests on clearly defined standards. Without criteria, evaluating possible solutions becomes arbitrary. With criteria, the process becomes analytical and defensible.
The DECIDE Model in Nursing demonstrates that structured evaluation enhances clinical judgment and reduces the likelihood of error. By explicitly identifying benchmarks related to patient-centered priorities, clinical guidelines, ethical responsibilities, and resource realities, practitioners strengthen accountability and promote safe outcomes.
Ultimately, establishing the criteria within the DECIDE Model in Nursing transforms decision making from an intuitive act into a disciplined, systematic process. It ensures that decisions are made thoughtfully, transparently, and in alignment with professional standards. Through careful prioritization of risks, benefits, resources, and patient preferences, clinicians are better equipped to identify the best possible outcome and support high-quality patient care.
Identify the Best Alternative in the Decision-Making Model
Within the DECIDE Model in Nursing, once clinicians define the problem and establish the criteria, the next essential step of the decision-making process is to identify the best alternative. This stage requires deliberate analysis rather than intuition. It represents the point at which theoretical reasoning transitions toward actionable selection.
The DECIDE Model in Nursing emphasizes that choosing the best alternative is not about selecting the first acceptable option. Instead, it involves systematically evaluating a number of options against previously established criteria. This step ensures that effective decision making remains grounded in safety, ethics, patient-centered priorities, and evidence-based standards.
Identifying the best alternative is central to achieving effective decisions. If earlier stages of the decision-making process are analytical, this stage is evaluative and comparative. The quality of outcomes often depends on how carefully practitioners assess possible solutions before implementing the decision.
Techniques to Identify the Best Option Among Available Alternatives
Comparing Interventions
Comparative analysis is a foundational strategy within the DECIDE Model in Nursing. After generating possible solutions, clinicians must examine how each intervention aligns with established benchmarks.
For example, consider a patient with uncontrolled postoperative pain. Possible interventions may include:
- Increasing opioid dosage
- Introducing non-opioid adjuncts
- Implementing non-pharmacologic strategies such as repositioning or relaxation therapy
Using the DECIDE Model in Nursing, each option is evaluated systematically:
- Does it meet safety criteria?
- Does it align with patient preferences?
- Does it reflect current clinical guidelines?
- Are there contraindications?
This structured comparison allows the decision maker to move beyond convenience and toward rational analysis. By comparing interventions side by side, clinicians reduce variability in how decisions are made and enhance accountability.
Risk-Benefit Analysis
Risk-benefit analysis is a critical tool for identifying the best alternative. In healthcare, nearly every intervention carries potential benefits and possible adverse outcomes. Effective decision-making requires weighing these elements carefully.
For example, initiating anticoagulation therapy in a patient with atrial fibrillation reduces stroke risk but increases bleeding risk. The DECIDE Model in Nursing encourages structured evaluation of:
- Magnitude of benefit
- Probability of harm
- Patient-specific risk factors
- Urgency of intervention
Through systematic reasoning, the clinician determines whether the anticipated benefits outweigh the risks. This balanced assessment strengthens effective decisions and reduces the likelihood of unintended consequences.
Risk-benefit analysis also reinforces ethical responsibility. Decisions are made transparently, and the reasoning behind selecting the best course of action can be justified if questioned.
Evidence Appraisal
Evidence appraisal ensures that chosen interventions are supported by credible research and clinical standards. Within the DECIDE Model in Nursing, selecting the best alternative requires integrating evidence-based practice into the decision-making process.
Evidence appraisal involves:
- Reviewing current guidelines
- Assessing the quality of research
- Considering relevance to the patient’s condition
- Evaluating consistency of findings
For example, in managing hypertension, clinical guidelines may recommend lifestyle modification as first-line therapy before initiating medication in certain populations. By appraising evidence, clinicians make informed decisions that align with best practice rather than outdated habits.
Research consistently demonstrates that evidence-based approaches improve patient outcomes and reduce practice variability (Melnyk & Fineout-Overholt, 2019). The DECIDE Model in Nursing integrates this appraisal process to strengthen the reliability of decisions made.
Clinical Reasoning Strategies for Choosing the Best Course of Action
Critical Thinking Frameworks
Critical thinking is essential for navigating complex decisions. Within the DECIDE Model in Nursing, structured reasoning frameworks guide practitioners in analyzing information logically and systematically.
Critical thinking involves:
- Identifying assumptions
- Recognizing patterns in patient data
- Anticipating potential complications
- Reflecting on previous experiences
For example, when managing a patient with sepsis, clinicians must rapidly interpret laboratory values, vital signs, and clinical presentation. The DECIDE Model in Nursing supports a systematic approach, ensuring that the decision-making process remains organized even in urgent situations.
Structured reasoning strengthens professional judgment and ensures that decisions are not based solely on routine or familiarity.
Avoiding Cognitive Biases
Cognitive biases can distort judgment and lead to making the wrong decision. Common biases include:
- Anchoring bias (fixating on initial impressions)
- Confirmation bias (seeking evidence that supports preexisting beliefs)
- Availability bias (relying on recent experiences rather than objective data)
The DECIDE Model in Nursing mitigates these biases by requiring deliberate progression through each step of the decision-making process. By systematically comparing alternatives and evaluating criteria, clinicians reduce the influence of subjective shortcuts.
For example, assuming that a young patient’s chest pain is anxiety-related without evaluating cardiac markers reflects anchoring bias. Using a structured approach ensures comprehensive assessment before identifying the best course of action.
Research on diagnostic reasoning emphasizes that systematic models reduce cognitive error and enhance clinical safety (Croskerry, 2009). The DECIDE Model in Nursing embodies this systematic reasoning process.
Collaborative Decision Making
Complex decisions often benefit from interdisciplinary collaboration. The DECIDE Model in Nursing supports collaborative decision making by encouraging discussion of alternatives with physicians, pharmacists, therapists, and other healthcare professionals.
For instance, managing a patient with multiple comorbidities may require consultation to determine medication adjustments. Collaboration enhances the decision-making process by incorporating diverse expertise and perspectives.
Shared reasoning:
- Expands the number of options considered
- Improves risk assessment
- Strengthens ethical accountability
- Enhances patient-centered outcomes
Through collaborative dialogue, clinicians make informed choices that reflect collective expertise rather than isolated judgment.
Integrating Selection into the Broader Decision-Making Process
Identifying the best alternative represents a pivotal moment in the DECIDE Model in Nursing. It is the stage where analysis transitions into commitment. However, selection does not occur in isolation. It remains connected to previously established criteria and must be followed by careful implementation and evaluation.
By systematically comparing interventions, conducting risk-benefit analysis, appraising evidence, applying critical thinking frameworks, avoiding cognitive biases, and engaging in collaborative decision making, practitioners strengthen effective decision making across clinical settings.
Develop and Implement a Plan of Action in Nursing Practice
Once the best alternative has been identified within the DECIDE Model in Nursing, the next critical step of the decide model is to develop and implement a plan of action. This stage transforms abstract decision-making into tangible clinical interventions, ensuring that every action aligns with previously established criteria. In essence, this step bridges reasoning with practice, providing a structured pathway to achieve effective decisions and patient-centered outcomes.
Implementing a plan effectively requires attention to detail, professional accountability, and interdisciplinary coordination. The DECIDE Model in Nursing ensures that decisions are not only made but also executed safely, systematically, and in accordance with evidence-based practice.
How to Develop and Implement a Plan that Aligns with Established Criteria
The first principle of this stage is translating decisions into actionable steps. A clear plan converts theoretical choices into measurable interventions, timelines, and responsibilities. The plan should explicitly reference the criteria established in the previous step of the DECIDE Model in Nursing, including patient safety, clinical guidelines, ethical standards, and patient preferences.
For example, consider a patient with acute exacerbation of chronic obstructive pulmonary disease (COPD). The plan may involve oxygen therapy, bronchodilator administration, and monitoring for complications. Each step corresponds to established criteria: improving oxygenation, adhering to protocols, and mitigating risk. Without a structured plan, even well-considered decisions may fail in practice due to poor execution or lack of accountability.
Delegation and Interdisciplinary Collaboration
Developing a plan of action often requires collaboration across healthcare disciplines. The DECIDE Model in Nursing emphasizes that effective implementation is rarely an isolated activity. Delegation ensures that interventions are carried out by team members with the appropriate skills, while interdisciplinary collaboration brings diverse perspectives to the plan.
For instance, managing a patient with diabetes and cardiovascular comorbidities may involve:
- Nurses monitoring blood glucose and administering medications
- Physicians adjusting pharmacological therapy
- Dietitians providing nutritional counseling
- Physical therapists supporting mobility and rehabilitation
By integrating collaborative decision making into plan implementation, the DECIDE Model in Nursing reduces errors, improves efficiency, and enhances patient outcomes.
Documentation Standards
Accurate documentation is a critical component of developing and implementing a plan. Within the DECIDE Model in Nursing, recording the rationale, actions taken, and outcomes ensures that the decision-making process is transparent and accountable. Documentation also provides a reference for future decisions, supports legal protection, and enhances communication among the care team.
For example, a nurse implementing a plan for postoperative pain management should document:
- Pain assessment scores
- Chosen interventions and rationale
- Patient response and effectiveness
- Adjustments made based on clinical evaluation
Consistent documentation ensures that decisions are made, implemented, and evaluated systematically, reinforcing safe and evidence-based care.
Practical Application: Using the DECIDE Model in Real Clinical Scenarios
Acute Care Example
In an intensive care unit, a patient presents with hypotension and altered mental status. Following the DECIDE Model in Nursing:
- Define the problem – Low blood pressure secondary to suspected sepsis
- Establish criteria – Stabilize vitals, prevent organ dysfunction, follow sepsis guidelines
- Identify the best alternative – Rapid fluid resuscitation, broad-spectrum antibiotics, and close monitoring
- Develop and implement a plan – Assign roles for fluid administration, lab monitoring, and medication delivery; document interventions; notify physicians
- Evaluate and monitor – Assess blood pressure response, urine output, and mental status continuously
This structured approach ensures timely intervention and reduces the risk of complications.
Community Health Example
In a public health setting, consider a clinic addressing rising rates of childhood obesity. Using the DECIDE Model in Nursing:
- Define the problem – Increasing prevalence of obesity-related conditions
- Establish criteria – Promote healthy lifestyle, ensure accessibility, and engage families
- Identify the best alternative – Implement nutrition education, physical activity programs, and community outreach
- Develop and implement a plan – Coordinate with dietitians, school staff, and community leaders; schedule workshops; provide educational materials
- Evaluate and monitor – Track participation, BMI trends, and behavioral changes in children
Structured planning allows interventions to be measurable and aligned with community needs.
Leadership/Management Example
In a hospital management scenario, a nurse manager identifies high rates of staff turnover. Applying the DECIDE Model in Nursing:
- Define the problem – Staff dissatisfaction leading to attrition
- Establish criteria – Improve retention, enhance morale, optimize scheduling
- Identify the best alternative – Revise shift rotations, provide professional development, and implement mentorship programs
- Develop and implement a plan – Assign responsibilities, establish timelines, and communicate goals with staff
- Evaluate and monitor – Track retention rates, staff satisfaction surveys, and performance metrics
By structuring the decision-making process, the manager ensures interventions are deliberate, measurable, and sustainable.
Integrating Planning into the DECIDE Model
The DECIDE Model in Nursing emphasizes that developing and implementing a plan is more than executing a single intervention—it is about translating informed choices into actionable steps while maintaining accountability and adherence to established criteria. Effective plans anticipate obstacles, include delegation strategies, integrate evidence-based practice, and prioritize patient-centered outcomes.
Through structured planning, the DECIDE Model in Nursing ensures that decisions are not only made but also executed successfully, setting the stage for the subsequent step: evaluating and monitoring outcomes. In doing so, the model provides a clear framework for translating reasoning into practical, measurable action across diverse healthcare settings.
Evaluate and Monitor Outcomes for Continuous Improvement
The final step of the DECIDE Model in Nursing focuses on evaluating and monitoring outcomes to ensure that decisions achieve their intended goals and to facilitate continuous improvement in clinical practice. This stage is essential because even well-conceived plans of action may require refinement when applied in real-world settings. Evaluation allows nurses to determine whether interventions meet established criteria, whether patient safety is maintained, and whether the desired health outcomes are achieved.
Within the DECIDE Model in Nursing, evaluate and monitor emphasizes both systematic observation and reflective reasoning. This step reinforces accountability, strengthens clinical judgment, and ensures that every decision made is both effective and evidence-based.
How to Evaluate and Monitor the Effectiveness of Clinical Decisions
Outcome Measurement Indicators
Effective evaluation begins with the selection of outcome measurement indicators. These are specific, quantifiable parameters used to determine the success of the implemented plan. Indicators should reflect both patient-centered priorities and professional standards.
For example, in a patient recovering from surgery, relevant indicators may include:
- Pain scores and analgesic effectiveness
- Wound healing progress
- Vital signs stability
- Mobility milestones
In the context of community health interventions, outcome indicators could include:
- Vaccination coverage rates
- Reduction in disease incidence
- Patient adherence to treatment plans
By using structured indicators, the DECIDE Model in Nursing ensures that monitoring is objective, measurable, and linked directly to the best course of action previously selected.
Patient Response Assessment
Evaluating patient response is a key element of monitoring outcomes. The DECIDE Model in Nursing stresses that make informed decisions requires ongoing assessment of how interventions impact the patient.
For instance, if a patient with heart failure receives diuretic therapy, clinicians should monitor:
- Fluid balance and weight changes
- Electrolyte levels
- Blood pressure and heart rate
- Symptom relief, such as reduced edema or dyspnea
Direct observation and patient feedback help the decision maker determine whether the plan is achieving the desired outcomes or requires adjustment. Patient-centered assessment aligns interventions with individual needs, reinforcing the structured, systematic approach embedded in the DECIDE Model.
Safety Monitoring
Safety monitoring is an indispensable component of evaluate and monitor. Even interventions with strong evidence may carry risks or unintended consequences. Within the DECIDE Model in Nursing, continuous monitoring ensures that adverse events are detected early, and appropriate corrective measures are implemented promptly.
For example:
- In pharmacologic therapy, monitoring for side effects such as hypotension, bleeding, or allergic reactions
- In mobility interventions, observing for falls or injuries
- In infection control, tracking signs of hospital-acquired infections
Integrating safety checks into evaluation supports effective decision-making, minimizes harm, and strengthens accountability in clinical practice.
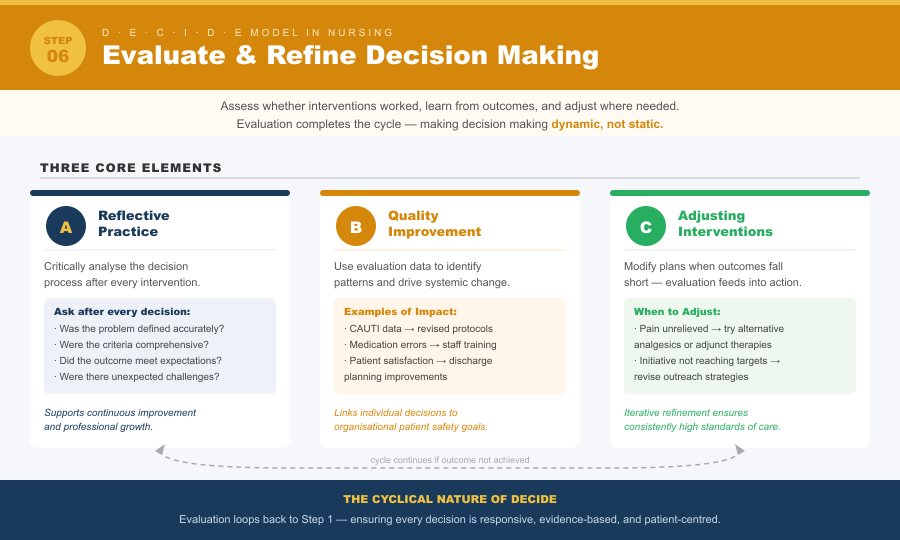
How to Evaluate the Decision and Refine Future Decision Making
Reflective Practice
Reflective practice is central to refining decisions and improving future outcomes. After evaluating interventions, nurses should critically analyze the decision-making process, considering:
- Was the problem defined accurately?
- Were the criteria appropriate and comprehensive?
- Did the selected alternative achieve the desired outcome?
- Were there unexpected challenges or errors?
Reflective practice encourages learning from both successes and shortcomings. For example, if a postoperative pain management plan only partially relieves discomfort, reflection may reveal gaps in assessment, patient communication, or intervention timing. The DECIDE Model in Nursing incorporates this reflective step to support continuous improvement and professional growth.
Quality Improvement
The evaluation process also informs broader quality improvement initiatives. Data gathered during monitoring can identify patterns, highlight areas for systemic enhancement, and support evidence-based policy adjustments.
For example:
- Monitoring catheter-associated urinary tract infections (CAUTIs) may lead to revised insertion protocols
- Evaluating medication error incidents can inform staff training and workflow changes
- Reviewing patient satisfaction outcomes may guide adjustments in discharge planning
Through structured evaluation, the DECIDE Model in Nursing links individual clinical decisions to organizational improvement and patient safety outcomes.
Adjusting Interventions When Necessary
Even carefully implemented plans may require modification. The DECIDE Model in Nursing ensures that evaluation feeds directly into action. If patient response, outcome indicators, or safety monitoring reveal suboptimal results, the decision maker can adjust interventions to realign with established criteria.
For example:
- A patient not responding to initial pain management may require alternative analgesics or adjunct therapies
- A community health initiative failing to reach targeted populations may need new outreach strategies
- Staffing or workflow interventions in a hospital unit may be adjusted to optimize efficiency and patient care
This iterative process reinforces a step-by-step guide approach, where decisions are continuously assessed, refined, and improved, ensuring high standards of care.
Integrating Evaluation into the DECIDE Model
Evaluation and monitoring complete the cyclical nature of the DECIDE Model in Nursing, linking problem identification, criteria establishment, selection of alternatives, and implementation to measurable outcomes. By systematically assessing the effectiveness of decisions, reflecting on processes, and adjusting interventions as needed, the model fosters continuous improvement, reduces errors, and enhances overall patient outcomes.
The DECIDE Model thus ensures that decision making is not static but dynamic, responsive to patient needs, and aligned with professional and ethical standards. It reinforces that every decision is part of a structured approach designed to optimize safety, effectiveness, and quality in nursing practice.
Conclusion
The DECIDE Model in Nursing offers a structured, systematic framework for effective decision making across diverse clinical settings. By guiding clinicians through a step-by-step process—from accurately defining the problem, establishing criteria, identifying the best alternative, to developing and implementing a plan, and finally evaluating outcomes—the model transforms complex clinical judgments into actionable, evidence-based decisions. Each stage emphasizes patient-centered priorities, safety, ethical considerations, and accountability, ensuring that interventions align with both professional standards and individual patient needs.
Using the DECIDE Model in Nursing not only reduces the risk of errors and enhances patient safety but also cultivates reflective practice, critical thinking, and collaborative decision making. Its systematic approach empowers clinicians to make informed choices, weigh risks and benefits, and adjust interventions based on measurable outcomes. Across acute care, community health, and leadership contexts, the model demonstrates its versatility as a decision-making tool that bridges theory and practice.
Ultimately, the DECIDE Model is more than a procedural guide—it is a structured approach to clinical reasoning that fosters consistency, transparency, and continuous improvement. By integrating the model into everyday nursing practice, healthcare professionals can navigate complex decisions confidently, optimize patient outcomes, and uphold the highest standards of nursing care.
Frequently Asked Questions
What is the DECIDE Model in Nursing?
The DECIDE Model in Nursing is a structured decision-making tool that guides nurses through a systematic, step-by-step process to make informed and effective clinical decisions. It emphasizes defining the problem, establishing criteria, identifying the best alternative, developing and implementing a plan, and evaluating outcomes, ensuring safety, accountability, and patient-centered care.
What are the 5 stages in Benner’s Model?
Patricia Benner’s Novice to Expert Model describes five stages of nursing proficiency:
- Novice – Beginner with no experience, follows rules rigidly.
- Advanced Beginner – Gains experience, recognizes recurring situations.
- Competent – More deliberate planning, efficient problem-solving.
- Proficient – Holistic understanding, anticipates needs, sees the bigger picture.
- Expert – Intuitive grasp of situations, highly skilled clinical judgment.
What is the Decision-Making Model in Nursing?
A Decision-Making Model in Nursing is a systematic framework that helps nurses analyze clinical situations, weigh alternatives, and implement solutions. Models like DECIDE or clinical reasoning frameworks support effective decision making, reduce errors, and integrate evidence-based practice into patient care.
What are the six steps of the DECIDE Model in order?
The six steps of the DECIDE Model in Nursing are:
- D – Define the problem
- E – Establish the criteria
- C – Consider the alternatives (Identify the best alternative)
- I – Identify the best option
- D – Develop and implement a plan
- E – Evaluate and monitor the outcomes
